Cause Exploration Prizes: Could New Technology Help Solve the Glasses Problem?
This essay was submitted to Open Philanthropy’s Cause Exploration Prizes contest and posted to the Forum with the author’s permission.
Summary of the problem
There are 2.2 billion people in the world who are visually impaired. There are two main causes of visual impairment. The first is medical problems, such as cataracts or vitamin A deficiency, which require surgery or medical treatment to treat them. The second is refractive errors, which means that the eyes are healthy, but the person needs glasses in order to see clearly. Uncorrected refractive errors (URE) are the leading cause of visual impairment worldwide. In 2020, more than 1.1 billion people in the world were visually impaired simply because they did not have access to glasses, and this number is expected to rise to 1.8 billion by 2050. This essay will focus on addressing URE, barriers to providing glasses, and new technology that might greatly expand the scope of care.
Refractive errors, such as myopia, hyperopia, astigmatism, and presbyopia, are easily corrected with glasses. Refractive error is an extremely common problem; 75% of American adults wear glasses or contact lenses for correction. In high-income nations, the incidence of visual impairment from uncorrected refractive errors (URE) is less than 10%, since most people have access to glasses through their medical insurance. However, the burden of visual impairment from URE is more than four times greater in low- and middle-income countries compared to high-income countries. In western, eastern and central sub-Saharan Africa, 80% of the population suffers with uncorrected refractive errors.

While the global incidence of blindness has decreased in the past 30 years due to improvements in medical treatments of trachoma and river blindness, this has been offset by the increasing age of the population. There has been a shift from medical visual impairment to refractive visual impairment as the leading cause of disability. Presbyopia, which is the need for reading glasses or bifocals, develops in 100% of people by the age of 50. Without reading glasses or bifocals, people over age 50 cannot perform tasks requiring near vision, such as reading, removing pebbles from beans or rice, or spotting holes in their malaria bed net.
There are 826 million severely impaired and 1.8 billion moderately impaired people who need, but do not have access to reading glasses, which would allow them to easily perform these tasks. This includes up to 94% of the population in some countries in Africa and Asia. (6, 19)
Importance of solving the problem
Disability
URE is the number one global cause of disability.(4) According to the Global Burden of Disease 2013 study, the global burden of URE was 11.3 million disability-adjusted life years (DALYs). The number of DALYs increased 43% from 1990 to 2013. Highest DALYs (241 DALYs per 100,000) were found in low-income areas, including southeast Asia, eastern Mediterranean, and Africa. Women over the age of 40 had higher DALYs from URE compared to men and younger people. Older people had higher DALYs which increased with age. URE burden is inversely proportional to a country’s Human Development Index, so countries with the least-developed health and education provisions were more affected by URE.(5)
Morbidity
URE is not just about inability to work. Because vision is the dominant of the five senses, people fear blindness more than many lethal conditions such as cancer. Mobility and autonomy are usually dependent on vision. URE is a tremendous hurdle to education, literacy, workforce participation, and social connectedness. People with visual impairment are more likely to be unemployed, depressed, or suffer from violence or accidents. (11) For older adults, visual impairment is associated with increased incidence of falls, hip fractures, decreased autonomy, and social isolation.(12) In addition, URE impacts not only the patient, but also their family members who must care for them physically and emotionally. (13) Elderly people with visual impairment are more likely to lose ambulatory skills and daily activities of living, and need nursing care earlier than sighted counterparts. Visual impairment also hastens the onset of dementia. (16, 17)
URE impacts children even more strongly. Between three and five percent of children have medical conditions such as strabismus (crossed eyes) or amblyopia (lazy eye) which must be treated with glasses at a young age. If left untreated, these conditions can cause permanent loss of vision, disfigurement, and loss of depth perception by the age of 10 years. Utility analysis of patients with amblyopia and strabismus show decreased utility throughout adulthood. On survey, 70% of patients with amblyopia or strabismus would be willing to exchange lifetime years for perfect vision. (15)
Financial costs to societies
The annual global productivity loss from URE from myopia and presbyopia was US $269 billion (9). This is an underestimate of total URE cost, because the two other types of refractive error, astigmatism and hyperopia, were not included. In addition, as the global population continues to age, the incidence of presbyopia continues to increase each year. (7) In some countries in Southeast Asia, annual productivity loss from URE was equivalent to more than 1% of gross domestic product (8). Global productivity loss also does not consider secondary health costs, such as falls and hip fractures or depression secondary to visual impairment, or the cost to families, such as family members leaving the workforce to care for visually impaired people. Finally, URE exacts an extreme toll on children and adolescents who drop out of school due to URE, potentially losing a lifetime of productivity.
Neglectedness
Preventing blindness is a popular public health topic, and therefore does not seem particularly neglected. URE is always lumped in together with all forms of blindness, including medical and surgical conditions such as cataracts and macular degeneration. There have been numerous calls to action for all countries to implement essential eye care, including medical and surgical eye care, for everyone. However, these ambitious plans never seem to make a dent in the current prevalence of URE. To the credit of many hardworking people, there has been tremendous improvement in several medical forms of blindness, such as river blindness, trachoma, vitamin A deficiency, and cataracts. Some forms of treatment, such as cataract surgery, have high costs per patient, and are much less cost-effective compared to URE. Other conditions, such as macular degeneration, are very difficult to treat, require medications, and generally do not improve the vision.
Who is working on the problem?
International organizations calling for expanded healthcare
“Vision 2020: the right to sight” was an international conference held in 1999, which resulted in four advocacy plans, plus a World Health Organization action plan which called for universal access to eye care and a 25% reduction in URE by 2019. Later, in 2007, the World Congress on Refractive Error met and passed the Durban Declaration, which specifically called for governments and industry to prioritize URE and meet the Vision 2020 goals. But in 2020 there were still 1.1 billion people visually impaired from URE – an increase from previous years. In 2021, the United Nations adopted the “Vision for Everyone” sustainable development goal, which aims to provide eye care for all people by 2030. However, significant disparities in access continue to exist despite these efforts. Most global advocacy involves providing eye care through the country’s government-provided health services, but these services have likely been overwhelmed by more pressing and complex problems, such as HIV, tuberculosis, malaria, malnutrition, infant mortality, and Covid-19. In addition, the global burden of URE keeps rising, due to the aging population.
Philanthropic organizations
Private charities such as OneSight and Eyes on Africa provide glasses for patients with URE. OneSight has established permanent community vision clinics in Gambia, which train and employ local citizens to examine patients and make glasses. OneSight collects US $15 million annually, and serves 53 countries in Africa, rural China, India, southeast Asia, South America. These clinics are staffed by local optometrists who perform comprehensive exams and refractions on patients.
Eyes on Africa is unique because it does not utilize optometrists to perform eye exams. Instead, Eyes on Africa distributes off-the-shelf, one-prescription-fits-all reading glasses, similar to what one might purchase over-the-counter. This is very cost-effective, because these over-the-counter glasses actually help a very large percentage of people over the age of 40, and they are very inexpensive, less than US $1. Eyes on Africa does not provide its financials on its website, but it appears to be a small, grassroots organization.
There are many other eye care charities which focus on the medical and surgical treatment of eye conditions, especially cataracts. Some of these charities also provide glasses, but since they focus on surgery, they serve a smaller number of patients. Charity Vision and Cure Blindness provide cataract surgery and glasses to patients in India, Africa and southeast Asia. Eyes for Africa (unrelated to Eyes on Africa) provides cataract surgery in Ethiopia.
There are several companies which provide glasses for charity. Luxottica provides glasses for OneSight, and DIFF Eyewear provides glasses for Eyes on Africa.
There are dozens of charities who collect used eyeglasses in the US and ship them to Africa and southeast Asia. Lion’s Club, Salvation Army, Goodwill, Warby Parker, ReSpectacle and many more charities run extremely popular programs collecting used eyeglasses for donation; however, only a tiny fraction of these glasses can be used, since each patient needs a customized glasses prescription. Each pair of donated glasses must be read by special machinery (to determine the lens prescription) and labeled, then matched to a patient with a similar prescription and face size, a task which must be performed by an optometrist. The chances of matching a pair of used glasses to a patient are near zero. Due to the enormous burden of skilled labor needed to sort through and match used glasses, this type of program is extraordinarily low-yield and should be discouraged.
Tractability
URE is a highly tractable problem. Glasses provide instant, dramatic improvement in vision, without adverse effects. Most glasses can last for many years of use. Custom glasses can be produced inexpensively, and are widely sold in many countries for US $7. Over-the-counter reading glasses, such as those distributed by Eyes on Africa, are available in several standard prescriptions for less than US $1. Given that there are 826 million adults with presbyopia who need over-the-counter reading glasses, plus 120 million people who need custom glasses for myopia or astigmatism, the financial cost of the glasses would be US $1.66 billion. (7) Since the estimated annual decrease in productivity due to URE is US $269 billion annually, then if each person keeps the glasses that they receive for 5 years, the financial return for the glasses is 1,134x.
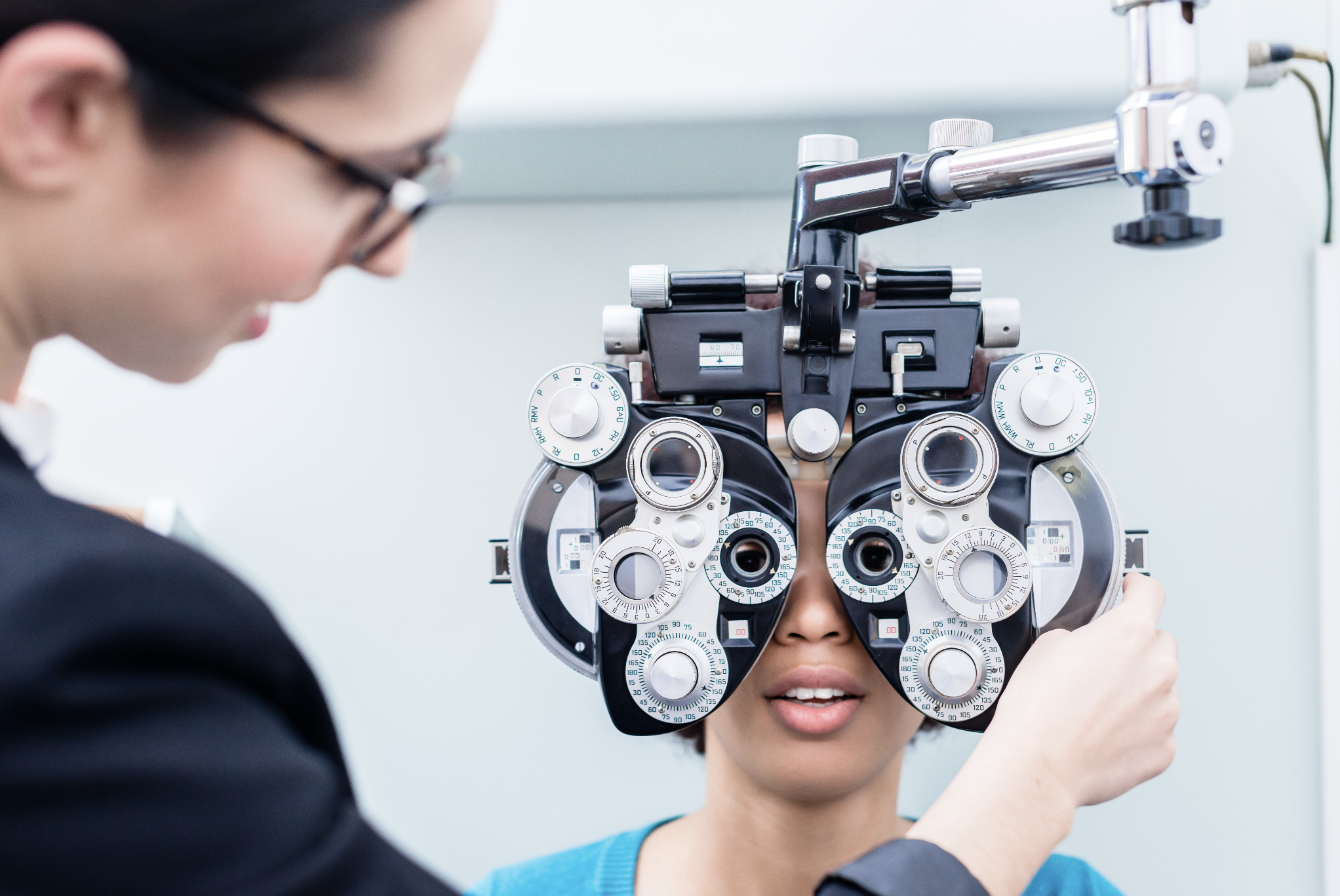
One significant limitation in providing glasses is the skilled labor requirement for refraction (determining the glasses prescription) for each patient. For people in developed countries, getting glasses means going to visit an optometrist or ophthalmologist in their medical office. These eye care professionals use high-tech autorefractor machines, which can give a close approximation of a patient’s glasses prescription as a starting point. This is then followed by a quick manual refraction to fine-tune the glasses prescription. In manual refraction, the doctor puts different eyeglass lenses over the patient’s eyes and asks them to choose which lens is clearer. (Which lens looks clearer, number one or number two?). If the patient has already had autorefraction, then the manual refraction just takes a minute to verify the prescription. The glasses lenses are then custom-made to the exact prescription in an optical shop. This exam requires skilled labor of an optometrist, plus the use of specialized, expensive autorefractor machine.
To provide vision services to underserved or remote locations, most organizations rely on makeshift clinics or “vision van” mobile services. Because most autorefractors are not portable, and require A/C power, mobile clinics usually rely solely on manual refraction. Performing manual refraction, without an autorefractor measurement as a starting point, requires much more of the optometrist’s time, usually 20 minutes per person. Because manual refraction relies heavily on patient participation in choosing which lenses improve their vision, any language barriers or cognitive issues greatly hamper manual refraction, in some cases rendering the refraction impossible. There is one commercially available portable autorefractor, but it is expensive (US$15,000), requires significant training and patient participation to use, and lasts only 80 minutes until it requires recharging.
Given that each optometrist can only screen perhaps 20 patients per day with manual refraction, this creates a bottleneck to providing glasses. Finding a way for a layperson to be able to determine each patient’s refraction would greatly enhance tractability.
In the past five years, a new technology called photoscreening has gained widespread use. Photoscreening machines are used in high-income countries to screen young children for refractive errors that might cause amblyopia (lazy eye). Advanced photoscreening machines such as the Welch Allyn/Hillrom Spot take only two seconds to measure a patient’s refraction and display it on the screen. Because photoscreening devices are designed to be used by laypeople for mass screening events, they are quick, portable, easy to use, and can refract hundreds of people before requiring recharging. In contrast to manual refractions and standard autorefraction, which require the patient to understand and follow complicated instructions, photoscreening does not require patient participation, beyond looking at the target for 2 seconds. This removes the language and cognitive barriers to care.
Because photoscreening requires no special skills, a layperson could refract hundreds of patients daily and therefore triage the patients. The machine has adjustable parameters that can be set to determine which patients need to see the optometrist for custom glasses, and which patients can simply be treated with over-the-counter $1 reading glasses. The optometrist or ophthalmologist on site could then focus only on the patients who failed the photoscreening test.

Photoscreening is performed with the user and the patient standing three to six feet apart, which is preferable for minimizing exposure to communicable diseases. No contact is required between the user and patient. This is in contrast to manual refractions or standard autorefraction, in which the patient’s face touches the machine, and the doctor and patient have their faces in very close proximity for several minutes.
Limitations of photoscreening
Photoscreening machines are only approved by the FDA for screening purposes, and not for use as autorefractors. Use of these machines for refractions would therefore be off-label, and there could be liability issues. However, most doctors find that the photoscreener refractions are highly accurate. In clinical trials, the Spot photoscreener had a 97% success rate (in measuring patients’ refractions), and a 90% specificity (in identifying patients who needed glasses). (10) During the Covid lockdown in 2020, when optometry and ophthalmology offices were under forced closure, many children were prescribed glasses using their Spot photoscreening results. These glasses have since been verified and the prescriptions are overwhelmingly correct.
One bias that photoscreening devices may have is that they were developed largely in Europe and the United States, and most accuracy studies have been performed on white children. There is a tendency of the Spot photoscreener to overestimate myopia and astigmatism in young children with very dark eyes, especially Asian and Black children. This is a significant concern since many countries with high levels of URE involve these populations. However, this overestimation problem affects all refractive machinery, and is not unique to photoscreeners. All optometrists are trained to compensate for this overestimation in young children during their training. For lay screeners, the parameters on the Spot can be adjusted to compensate.
Another problem with photoscreening is that as a screening device, it cannot fully replace a comprehensive eye examination by an optometrist (of course). For example, a patient may present with refractive error, which the photoscreener accurately diagnoses, but he may also have macular degeneration. Upon receiving the glasses, this patient only has a modest improvement in vision, and then would need to be referred to the optometrist for further evaluation. This is an acceptable trade-off in a utilitarian framework, because the patient was not harmed in any way – he was just inconvenienced in having to come to the eye clinic for a second visit. This problem is not unique to photoscreeners, and affects all autorefractors. But this problem elucidates the need for careful screening guidelines on which patients should be referred to optometry. These guidelines should be developed for each area, by a committee including public health professionals, optometrists and ophthalmologists, and operations managers, to minimize missing comorbidities.
The top photoscreening device, the Welch Allyn Spot, costs US $7500, about half the cost of a standard portable autorefractor. Although this price may preclude many underserved clinics from purchasing, since a very large number of patients can be quickly screened, the cost per-use is actually very low. Since photoscreeners allow laypeople to perform refractions, the optometrist is therefore freed of a very time-consuming burden, and can focus on patients with more difficult eye problems.
Pilocarpine
An alternative to glasses, pilocarpine 1.25% (Vuity) is a prescription eye drop medication that temporarily reverses presbyopia. The drop is used once daily in both eyes. In a randomized controlled clinical trial, patients with presbyopia treated with pilocarpine 1.25% were able to read without glasses.(14) Some patients developed transient headaches (14.9%, versus 9.4% with placebo) from the drops. Pilocarpine only improves presbyopia, and does not affect other refractive errors such as myopia or astigmatism. Pilocarpine can only be prescribed by an eye doctor, following a complete eye exam.
While pilocarpine 1.25%, which was the concentration studied in the clinical trial, is expensive (US $80 per month), similar concentrations of pilocarpine, such as 1% and 2%, cost more than four times less ($17 per month). This cost, however, is still much greater than the $1 over-the-counter reading glasses, which can last for many years, and don’t require eye exams, prescriptions, or follow up visits to an optometrist.
Possible interventions
International and government services
International organizations such as the World Health Organization and United Nations could encourage governments to focus more on URE. Most public policy is directed toward encouraging governments to provide comprehensive eye care for all, including full access to surgery and medical treatments. While this would be ideal, it is an overwhelming and unreasonable ask for a low-income country fighting to keep people from starving. Compared to surgery and most medical eye treatments, glasses are incredibly inexpensive, efficacious and cost-effective.
Ideally, every government would make the $1 over-the-counter reading glasses a priority for all people over the age of 40. While not perfect, this would be a significant improvement for 80% of the 1.8 billion people with presbyopia URE. Until governments can be persuaded to fund such projects, the best way is for charitable organizations to simply hand out over-the-counter reading glasses on a large scale in high-need areas. This could even be combined with other outreach areas. For example, organizations that currently distribute malaria bed nets could also give over-the-counter reading glasses to anyone over age 40. Anyone who has slept under a mosquito bed net understands the daily necessity of checking the net for holes – an impossible task for someone with uncorrected presbyopia. (20)
Glasses manufacturing
Manufacturing of glasses is infrastructure that every country should develop. Most over-the-counter reading glasses are mass-produced in factories by unskilled workers. Local manufacturing would provide jobs, decrease transportation and shipping costs, and decrease prices. Eventually, factories could be upgraded to produce custom eyeglasses from prescriptions.
Over-the-counter glasses for myopia
In areas such as southeast Asia, where myopia is a dominant refractive error, production of over-the-counter myopia glasses could make a drastic improvement in combating URE. Currently, the US has banned over-the-counter myopia glasses, likely because of fear of liability. People in the US with myopia must visit an optometrist to get custom glasses made. If $1 over-the-counter myopia glasses were available in America, no one would visit the optometrist, and people might choose the wrong strength and then have difficulty reading street signs when driving at night. However, liability aside, if there are millions of people in low-income countries with URE, whose vision could be improved by 90% by over-the-counter myopia glasses, then this would seem an obvious choice. Myopia is an especially pressing problem, since the incidence of myopia is increasing in epidemic proportions, particularly in Asia. (18) Production of over-the-counter myopia glasses would require examination of any laws or regulations that might prohibit their use. In addition, such glasses could not be exported to the US or Europe, where they are not allowed. It is likely that some of the factories which are already producing huge quantities of over-the-counter reading glasses for export could be adapted to produce myopia glasses instead. As a compromise to liability, over-the-counter myopia glasses could be distributed only through optometrists and eye clinics in high-need areas, instead of freely distributed like over-the-counter reading glasses.
Removing liability for photoscreeners to be used for glasses prescriptions
Large international and governing bodies could help exonerate the use of photoscreening machines as autorefractors in areas of need. From a utilitarian standpoint, a machine that allows millions of people with visual impairment due to URE to receive glasses should be allowed, even if the machine has not been formally evaluated as an autorefractor. Therefore liability should be excluded. Even if a patient receives glasses with a slightly incorrect prescription, there is no harm done to the patient, except that their vision could possibly have been corrected slightly better. In addition, governing bodies such as the National Eye Institute can help fund grants for the study of photoscreening devices as autorefractors.
Expansion of philanthropic reach
Probably the fastest way to expand the delivery of eye care services is to build up established organizations such as OneSight, which builds community eyeglass centers in high-need areas. Once these glasses centers are up and running, local governments may be more willing to absorb some of the costs to maintain them, particularly if someone else has already paid for the expensive machinery such as photoscreeners, vision vans for remote care, etc. OneSight currently does not have plans for expansion, likely due to their budget (US $15 million) and staffing limitations. However, providing the new photoscreening technology could streamline OneSight’s in-the-field operations, allowing laypeople to take over much of the burden of refracting patients. This would increase their capacity to see patients, probably by five to tenfold.
Currently, OneSIght appears to focus on providing comprehensive, individual eye exams, rather than mass screenings and handing out ready-made glasses. The implementation of photoscreeners and over-the-counter glasses for presbyopia and myopia would require OneSight to greatly expand its care and delivery models, employing far more laypeople and seeing many more patients. Whether this organization is open to such an expansion is unknown. It is possible that other organizations or government programs may be more suited to such high-level volume.
The authors have no relevant financial or non-financial conflicts of interest to disclose.
References
1) Swenor, B. Aging and Vision Loss: Looking to the Future. The Lancet GLobal Health, Volume 9, Issue 4, February 16, 2021.
2) Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years: evaluating the prevalence of avoidable blindness in relation to “VISION 2020: the Right to Sight”. Lancet Global Health 2020. doi.org/10.1016/S2214-109X(20)30489-7
3) Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Global Health 2020. doi: 10.1016/S2214-109X(20)30425-3
4) Holden BA. Uncorrected refractive error: the major and most easily avoidable cause of vision loss. Community Eye Health. 2007; 20: 37–39
5) Lou, L. Global patterns in health burden for Uncorrected Refractive Errors. Investigative Ophthalmology and Visual Science, Vol 57, November 2016.
6) (Reference missing in submission.)
7) World Report on Vision. World Health Organization, 2019.
8). Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology. 2015;122(8):1706–10.
9). Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, et al. Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis, and modeling. Ophthalmology. 2019;126(3):338–46.
10) Crescioni, M. Accuracy of the Spot and PlusOptix photoscreeners for detection of astigmatism. Journal of AAPOS. October 2015, volume 19, no. 5.
11) Evans JR, Fletcher AE, Wormald RP. Depression and anxiety in visually impaired older people. Ophthalmology. 2007;114(2):283–8.
12) Chew FL, Yong C-K, Ayu SM, Tajunisah I. The association between various visual function tests and low fragility hip fractures among the elderly: a Malaysian experience. Age and Ageing. 2010;39(2):239– 45.
13) Bambara JK, Wadley V, Owsley C, Martin RC, Porter C, Dreer LE. Family Functioning and Low Vision: A Systematic Review. Journal of Visual Impairment & Blindness. 2009;103(3):137–49.
14) Waring, G. The Gemini 1 Phase 3 Randomized Clinical Trial. JAMA Ophthalmology, March 2022, Volume 140, number 4.
15) Van de Graafe, E. Utility analysis of disability caused by amblyopia and/or strabismus in a population-based, historic cohort. Graefes Arch Clin Exp Ophthalmol. 2010; 248.
16) Bowen M, Edgar DF, Hancock B, Haque S, Shah R, Buchanan S, et al. Health Services and Delivery Research. The prevalence of visual Impairment in people with dementia (the PrOVIDe study): a cross sectional study of people aged 60-89 years with dementia and qualitative exploration of individual, carer and professional perspectives. Southampton (UK): NIHR Journals Library; 2016 July. 96.
17) Guthrie DM, Davidson JGS, Williams N, Campos J, Hunter K, Mick P, et al. Combined impairments in vision, hearing and cognition are associated with greater levels of functional and communication difficulties than cognitive impairment alone: Analysis of interRAI data for home care and long-term care recipients in Ontario. PloS One. 2018;13(2):e0192971.
18) Matsumura, S., Ching-Yu, C., Saw, SM. (2020). Global Epidemiology of Myopia. In: Ang, M., Wong, T. (eds) Updates on Myopia. Springer, Singapore.
19) Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, Naduvilath T, Naidoo KS. Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modeling. Ophthalmology. 2018 Oct;125(10):1492-1499. doi: 10.1016/j.ophtha.2018.04.013. Epub 2018 May 9. PMID: 29753495.
20) Vanden Eng JL, Mathanga DP, Landman K, Mwandama D, Minta AA, Shah M, Sutcliffe J, Chisaka J, Lindblade KA, Steinhardt L. Assessing bed net damage: comparisons of three measurement methods for estimating the size, shape, and distribution of holes on bed nets. Malar J. 2017 Oct 10;16(1):405. doi: 10.1186/s12936-017-2049-8. PMID: 29017537; PMCID: PMC5635507
Thanks to the authors for an excellent post! This is clearly an important problem. I wonder if it would be possible to estimate cost-effectiveness ($ per DALY averted) of some existing programs to norm this against global health and development causes currently favored by the EA community, such as GiveWell’s top charities?
What is the source for the claim that “Currently, the US has banned over-the-counter myopia glasses”? Glasses for mild myopia (up to about −4.0) are available without a prescription on Amazon (https://a.co/d/04RQUEk8 is the kind I wear when I take my contacts out), and AFAICT that is perfectly legal. AFAIK prescription lenses are only required for correcting more complex or multiple refractory problems like myopia+astigmatism, or myopia+presbyopia.
It seems like a highly neglected intervention to simply provide free myopia glasses in developing countries without expensive screening. If people put on a pair of them and it improves their vision, it shouldn’t require a professional to tell them to pick the weakest pair that seems to work and take them home to try.