How Can Engineers Do Impactful Work in Biosecurity?
This excerpt is taken from the High Impact Engineers’ Resources Portal, where we include an introduction to GCBRs and a list of resources and organisations. This was originally written by Bryce Rogers, who has since left HI-Eng to pursue other opportunities. We are grateful to WB, TA, JG, and JVB for their input and feedback. Any remaining mistakes are our own.
Edited 11th October 2023 to update links.
Unfortunately, there is probably no single “silver bullet” solution to reducing GCBRs or even just pandemics. To focus just on pandemics, experts posit that a comprehensive web of prevention, consisting of policy, technology, and public health measures ought to implemented. Physical technologies — face masks, medical devices, sanitisation systems, biosensors, manufacturing methods, and more — are critical to the efficacy of this web. Particularly valuable are technologies that are preventative (prevent rather than react to pandemics) and/or pathogen-agnostic (combat all/most pathogens, rather than a particular type or strain). Engineers are needed to develop and implement these technologies.
In their ambitious reports The Apollo Program for Biodefense and The Athena Agenda, the Bipartisan Commission on Biodefense (BCB) outlines several key technology areas they recommend to be developed and implemented to pandemic-proof the United States by 2030. We have selected and summarised some of the technology areas that are most relevant to engineers below (more in-depth discussions of each area can be found in the original reports).
Although far from comprehensive, if these technologies are developed and deployed successfully, they could be key elements in a global web of pandemic prevention. You can find many other concrete biosecurity project ideas here that we don’t cover below.
Next-generation personal protective equipment
Figure 2: Current personal protective equipment (PPE) leaves much to be desired. Photo by Matthias Heyde on Unsplash
Personal protective equipment (PPE), such as masks and respirators, creates a physical barrier between the wearer and pathogens. PPE has the potential to be an effective and pathogen-agnostic barrier against pandemics, but current designs leave much to be desired. In general, current designs are difficult to use properly, not widely accessible enough, don’t fit everyone, and haven’t been improved in decades. These could be improved by mechanical engineers and materials scientists.
There have been many projects to create next-gen PPE, such as the BARDA Mask Innovation Challenge, the XPrize Mask Challenge, and others both within and outside EA. Although there is a case for creating a new generation of improved PPE, it seems that the main bottleneck in this area is in generating an economic incentive to improve PPE, provided by changing policy or finding a non-healthcare market. More research is being done in this area (e.g. by Gryphon Scientific and others) so there is likely to be more clarity in this area in the coming year.
Pathogen transmission suppression in the built environment
The risk of pathogen transmission is generally vastly higher indoors than outdoors. Widespread incorporation of pathogen transmission mitigation technologies in highly populated buildings and vehicles could be an effective, pathogen-agnostic means of pandemic prevention. This would have the added benefit of passively decreasing the spread of non-pandemic diseases as well.
Although suppressing pathogen transmission indoors technically includes self-sterilizing materialsand fomite-neutralizing technologies (e.g. copper-alloy surfaces), the most promising interventions involve improving indoor air quality. The transmission of COVID-19 could be reduced by 80% with improved air filtration and indoor ventilation. The White House Office of Science and Technology Policy highlighted that clean indoor air is not only beneficial for reducing pandemic spread, but also mitigate the detrimental health effects of air pollution.
Figure 3: Increasing indoor air quality reduces not only pandemic spread but also air pollution. Photo by Álvaro Bernal on Unsplash
Improving indoor air quality can be achieved mechanically through 3 main technologies:
Improving ventilation
Improving filtration
Implementing ultraviolet germicidal irradiation (UVGI) – also known as germicidal UV (GUV)
Of these three technologies, we think that UVGI is the most promising intervention for engineers (particularly mechanical, materials, and aerospace engineers) to work on. You can explore the other ventilation and filtration in this and this EA Forum post.
Ultraviolet Germicidal Irradiation (UVGI)
UVGI interventions fall into two categories: conventional upper-room UVC and far-UVC.
Conventional upper-room UVC uses UV wavelengths of around 254 nm to disinfect the air in large indoor spaces. The UVC light is typically installed in the upper part of a room and directed upwards to kill airborne viral, bacterial, and fungal organisms. This method requires careful placement of the UVC emitters to prevent direct or reflected exposure to humans, as it can cause skin and eye damage. This technology was demonstrated in 1935 but still hasn’t been universally implemented, especially in LMICs. It is mainly constrained by the lack of skilled technicians available to install it properly, especially in resource-constrained countries. Read more on the US Center for Disease Control and Prevention website.
Far-UVC uses UV wavelengths between 207 and 222 nm in doses of 100 mJ/cm2 that have been proven effective at killing viruses and bacteria while being safe for human exposure. It is still an emerging technology and currently only used by early adopters in small-scale settings to disinfect surfaces and air. Although it is partly market/policy-bottlenecked, there are still many open questions around emitters and system design that lend themselves to engineering expertise. Organisations such as SecureBio and Rethink Priorities are looking into this area.
You can read more technical specifications for these two UVGI interventions in this GUV cheatsheet.
UVGI interventions can be combined with ventilation and/or filtration systems (attention to air flow and volume needed to ensure adequate irradiation time, among other considerations), and could also lend themselves to the integration of pathogen surveillance technologies. Africa CDC’s work in coordinating a continent-wide surveillance system to combat COVID-19 could be a model for other continents and nations. Technical work still needs to be done to develop pathogen surveillance technologies, which could potentially be a good fit for biochemists and chemical engineers.
Ubiquitous sequencing
Sequencing-based biosurveillance played a crucial role in detecting and tracking the spread of the COVID-19 pandemic. By sequencing the virus’s genetic material, researchers were able to understand the origins and evolution of the virus, identify and track the emergence of different variants, and assess the mutation’s influence on transmission, disease severity, or efficacy of vaccines against new strains. This helped public health officials make informed decisions about control measures, such as quarantine requirements and travel restrictions, to control the spread of the virus.
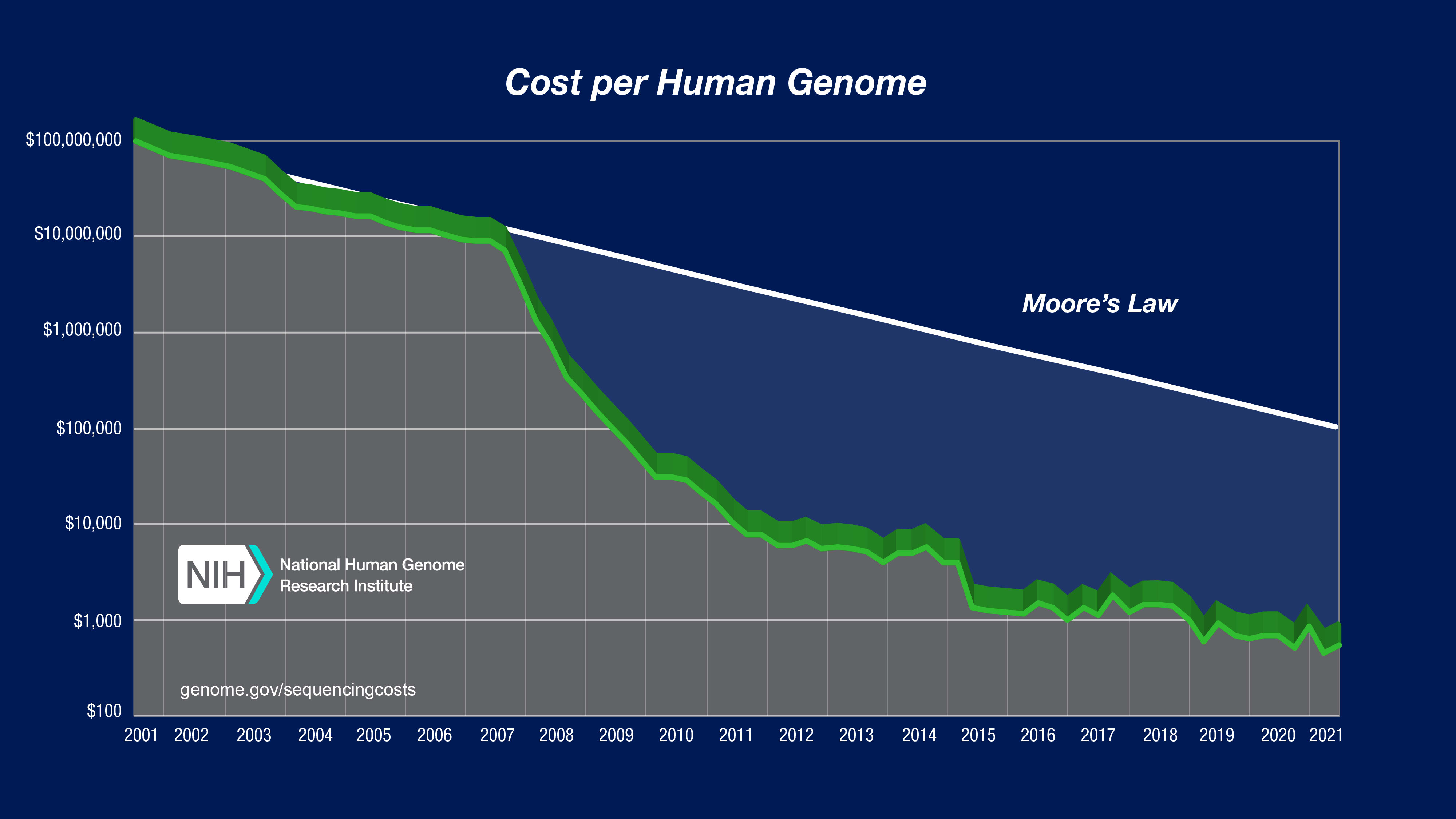
The cost of genetic sequencing has plummeted in recent decades, decreasing exponentially at a rate outpacing Moore’s law.
Figure 4: Exponentially decreasing cost of genetic sequencing in recent years (vertical axis is logarithmic)
This increasing affordability has enabled, in addition to many other advancements, more widespread application of metagenomic sequencing (the sequencing of all genetic material present in an environmental or patient sample). Unlike targeted sequencing, in which the genetic material of one or more specific pathogens is searched for in a sample, metagenomic sequencing enables rapid, pathogen-agnostic detection of potentially any disease present in the sample. Metagenomic sequencing for biosurveillance can be applied in two ways:
Metagenomics for environmental sampling involves the collection and analysis of genetic material from complex environmental samples, such as wastewater. Identification and characterisation of the microbes present in these samples can be used to monitor for dangerous pathogens or disease spread. Biobot Analytics and Concentric are companies doing wastewater monitoring and metagenomics for early detection.
Metagenomics for point-of-care clinical care allows the detection of a wide range of pathogens in human patients, including those that may not be detected by traditional culture-based methods. By rapidly identifying the specific cause of a disease, clinicians can quickly determine appropriate treatment options. The Respiratory Virus and Microbiome Initiative in the UK (along with other centres in the US and Germany) is developing metagenomic approaches to analyse respiratory swab samples.
The Bipartisan Commission on Biodefense advises that, to achieve the goal of ubiquitous metagenomic sequencing, sequencers should be made smaller, less reliant on expensive reagents, and to have on-chip sample preparation. The ideal outcome is for sequencers to be inexpensive and hand held. Reticula is one company pursuing this goal, and there are many others doing genetic sequencing.
Needle-free methods of drug and vaccine administration
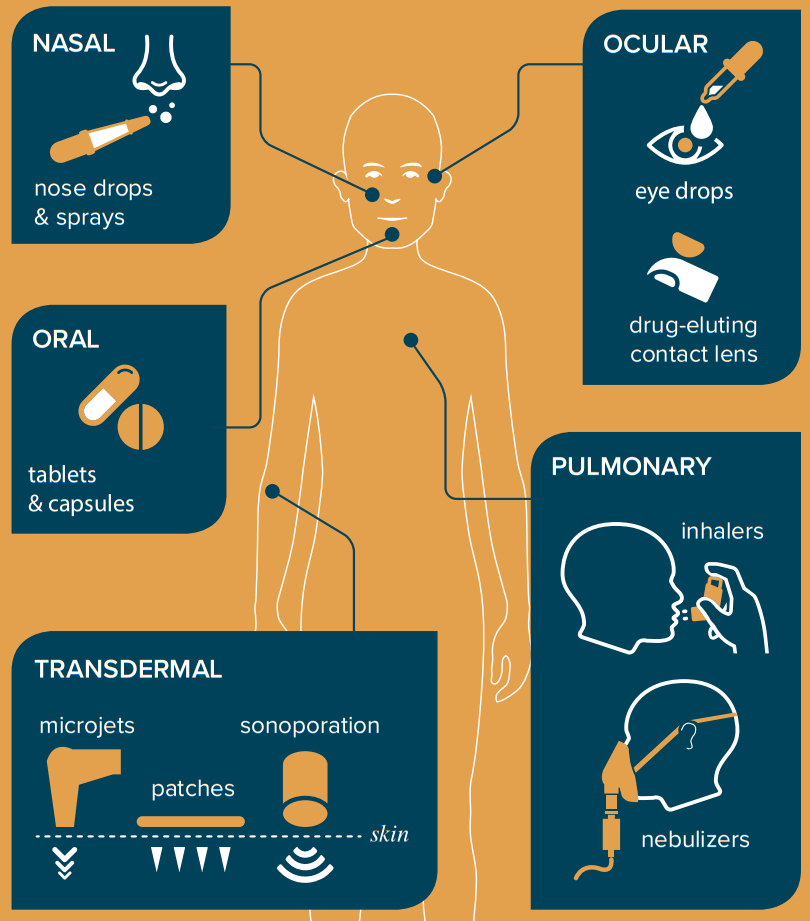
Most vaccines are administered via needle, the invasive nature of which necessitates administration by a healthcare provider. Needle delivery of vaccines thus adds to the already-severe strain on healthcare systems during pandemics. Additionally, fear of needles may decrease public uptake of vaccines that are only available via injection. Minimally-invasive self-administration methods could decrease strain on healthcare systems and maximise the number of individuals reached.
Many needle-free methods of drug and vaccine administration are being researched, including nasal sprays, contact lenses, oral capsules, inhalers, lasers, transdermal patches or microjets, and others. Biologists, engineers, and others are needed to bring these technologies to maturity such that they may be deployed during a pandemic.
Figure 5: Needle-free forms of drugs and vaccine administration (via the Athena Agenda)
Flexible and scalable manufacturing of pharmaceuticals
During a pandemic, the successful deployment of a novel therapeutic or vaccine requires rapid and large scale manufacturing. But many existing manufacturing methods are slow and difficult to repurpose to a novel pathogen. These problems might be addressed via increased use of platform technologies that use the same manufacturing processes for multiple different vaccines. This is typically achieved by encoding a therapeutic into genetic material — a process that could be rapidly repurposed and scaled during pandemic times.
Further work is needed to establish infrastructure that allows rapid large-scale vaccine manufacturing during outbreaks, and to mitigate current technical limitations of platform technologies, such as the reliance of mRNA vaccines on constant refrigeration. This area may be particularly relevant for industrial or manufacturing engineers.
Minimally- and non-invasive infection detection
Typically, an infection is only detected once a host has developed symptoms, gone to a healthcare provider, and had a pathogen-specific test administered. This is suboptimal during an outbreak given that symptoms may take days to develop, and the host may unknowingly infect several others before they receive a diagnosis. Ideally, a noninvasive, point-of-care and point-of-need testing technology capable of early detection could be deployed to individuals at risk of infection during an outbreak. Examples of point-of-care testing include pregnancy tests, lateral flow tests, and pooled next-generation sequencing. Policies to encourage testing at particular intervals, e.g. at schools, before large gatherings, would also be required.
Figure 6: Lateral flow tests for COVID-19 is an example of a point-of-care testing technology. However, the throat swab can be uncomfortable, and could be improved upon. Photo by Roman Wimmers on Unsplash
Statement on infohazards
An information hazard, or infohazard, is “a risk that arises from the dissemination of (true) information that may cause harm or enable some agent to cause harm.” An example of an infohazards in the context of biosecurity is the genetic sequence of a dangerous pathogen.
Some guidelines
Avoid brainstorming concrete attacks.
Focus on low-downside risk interventions, especially when developing interventions with dual-use potential. Upsides and downsides must be weighed carefully, and you can have a strongly negative impact when working on dual-use technology (it’s important to note that your impact does not zero out at ‘nothing’).
Consult with experts before taking actions.
Biosecurity is rife with infohazards, largely due to the dual-use nature of most biotechnological knowledge. For the interventions we explore above, the dual-use potential of indoor air interventions is close to nil; platform biotechnologies can vary a lot depending on the details of the platform; and biosurveillance could become a privacy and information security hazard. If you pursue biosecurity-adjacent work, it is important to deliberately prevent the dissemination of infohazards.



Great post and series, thanks!
Thank you!