[Cause Exploration Prizes] Why we should work on preventing suicide
This essay was submitted to Open Philanthropy’s Cause Exploration Prizes contest.
If you’re seeing this in summer 2022, we’ll be posting many submissions in a short period. If you want to stop seeing them so often, apply a filter for the appropriate tag!
Note from the author: This essay responds primarily to the “Cause-selection” prompt but also to the “measuring non-health, non-pecuniary benefits” prompt. I am going to start by discussing why suicide should be an important metric for worthwhile projects. But it is not a universal metric: some projects worth doing will not affect suicide rates, like improving air quality in Southeast Asia. That doesn’t mean they are not worthwhile. So suicide is not a universal metric—unlike DALYs, which can be used to assess most projects. In fact, the suicide rate metric is inextricably linked to a single cause. Once we accept the premise that suicide is a great metric, we must accept that we should be working on preventing suicides. And this pushes us immediately to look at certain kinds of projects and interventions. Suicide is both the metric and the cause.
Introduction—Suicide is both a metric and a cause
Every life has equal value, whether in the UK or in Sierra Leone, now or in 3022.
This value system lies at the core of effective altruist ideology—we should do our best to make more lives worth living, full of joy and hope, and free of pain and suffering.
But some lives are (subjectively) not worth living. For those 800,000 humans a year who choose to end their own lives, the goodness of life is not enough to outweigh their suffering. In this way, suicide is a revealed preference that, at least in their own perceptions, life was not worth living.
Preventing these lives from becoming so intensely painful is one of the clearest causes we could work on. Suicide is so simply bad, and preventing it is so simply good. This certainty should weigh strongly in favour of working to reduce suicide rates, compared to other measures of “good” that are more controversial.
An obvious comparison can be made to DALYs. Inherent in the use of DALYs is the assumption that disability makes your life slightly less worth living. For example, we assume that the baseline happiness of two people who are identical except that one is missing an arm, is different. While it may be reasonable to say that losing an arm is bad, and that disability can make life more difficult in various ways, it’s hard to get an accurate and universal measure of how disability affects the subjective experience of how good life is. By assuming that losing an arm reduces anyone and everyone’s life quality by (for example) 10%, we introduce noise into our DALY calculation. This should make us uncertain that DALYs accurately measure how people value their own lives. This is not the case for suicide. Suicide is a revealed preference that one’s life was subjectively not worth living. It is a crisp, clear measure of the negative value that someone might place on their own life.
Importance
How many lives are affected, and how much?
Suppose happiness is a scale from 0 to 100. At a level of 5 or below, people do not feel that their lives are worth living. We might expect people’s happiness levels to vacillate over time, with most people experiencing most levels. Many who dip below this critical level of 5 only remain there for a few hours, before returning to “life-is-worth-living” happiness levels. But when someone remains below this critical level for long enough, they start to consider means of suicide, and eventually may attempt and even succeed at killing themselves.
Under this model of happiness, suicide is the “tip of the iceberg”, revealing the existence of lives that, at one point in time, are so unhappy they are not considered worthwhile by those experiencing them. Of those who dip below the critical threshold of unhappiness, only some will stay there long enough to consider means. Of those who consider means, only some will attempt suicide. And of these, only some will successfully end their lives.
Figure 1: Suicide rates are a measurable underestimate of the number of critically unhappy people (not to scale)
Suicide is not a perfect metric for the thing we care about, which is the number of people who do not consider their lives worth living. But this is not necessarily a problem, because suicide rates are an underestimate of the number of lives subjectively not worth living.
There are about 800,000 suicides a year.[1]
For every person who successfully kills themselves, we can estimate that roughly 21 individuals attempt suicide.[2]
That’s 16.8 million people who attempt suicide annually.
For every person who attempts suicide, 2 more have had suicidal thoughts.
That’s 50.4 million people experiencing suicidal thoughts annually.
These 50.4 million are the people below this critical threshold of happiness. These are the people we really care about pushing above that line. These people are hard to measure. The figures I use above are based on surveys, where the phrasing of the question (e.g. “serious suicidal thoughts” vs. “suicidal ideation”) has a huge impact on estimates, alongside the biasing impact of social stigma. If it is embarrassing to admit you have had suicidal thoughts, you might lie.
Suicide rates, however, do not lie. They are an indicator of this underlying unhappiness that we should put huge effort into reducing and preventing.
There are two broad ways we can prevent suicide.
(a) We can reduce access to means
(b) We can push people above the critical threshold of happiness
By reducing access to means, we might prevent suicide, but we do not have any effect on people above the threshold. While it may delay the irreversible action that means it is too late for any other suicide prevention method to work, it does not fix the issue we care about—people not valuing their own lives.
If we focus instead on making those who would otherwise have killed themselves happier, we may have positive side effects on others.
We should care about the happiness of all people, beyond this group of extremely unhappy people who have suicidal thoughts. (Of course, we should care more about the people below the threshold, because their unhappiness is so great, and because suicide is an irreversible act which will prevent them from ever experiencing a life worth living.) Let us take the distribution of human happiness. On the left tail, we have those experiencing suicidal thoughts. By focusing on shifting these people to the right of the critical threshold, we may also have the indirect but welcome side effect of shifting some of the rest of the distribution right-wards. It seems likely that whatever intervention we use to prevent suicide, we will affect people above the critical threshold of happiness as well as those we are targeting below it. For example, suppose we intervene by improving some treatment for depression. This will notably affect those people with depression who might have killed themselves without this improved treatment. But people with depression who are above the “life is not worth living” threshold will also be affected. We might imagine in this case that we move the bottom half of the distribution right-wards, condensing the number of people around the mean. Thus, any positive impact we have on shifting those suicidal people above the critical threshold, should be multiplied by the (smaller) impact we are having on the rest of the distribution.[3]
Figure 2: By making critically unhappy people happier, we are probably making others happier too
So the goodness of suicide prevention may be multiplied by the indirect effects on the happiness of people across the rest of the distribution.
Suicide prevention work is likely to have other multiplier effects. Suicide harms the friends and family of those who take their lives. There is even evidence that being exposed to suicide increases your likelihood of taking your own life. Thus, any work to reduce suicide rates improves not only the lives of those who might kill themselves, it also prevents this harm rippling around those close to them.
Neglectedness
Suicide prevention is underfunded.
In the following, I will focus specifically on mental health funding, rather than funding for suicide prevention in general. But suicide prevention is broader than just mental health. For example, we might effectively work on suicide prevention by improving women’s rights, as discussed below. I have been unable to find data on wider work to prevent suicide, so will use mental health funding as a proxy for suicide prevention funding. I am comfortable using this proxy, as a large part of suicide prevention will be through mental health work, given the strong link between suicides and mental health disorders. Depending on the source (see links), between 46% and 90% of those who commit suicide have a known mental health condition.
Mental health is underfunded relative to other physical diseases.
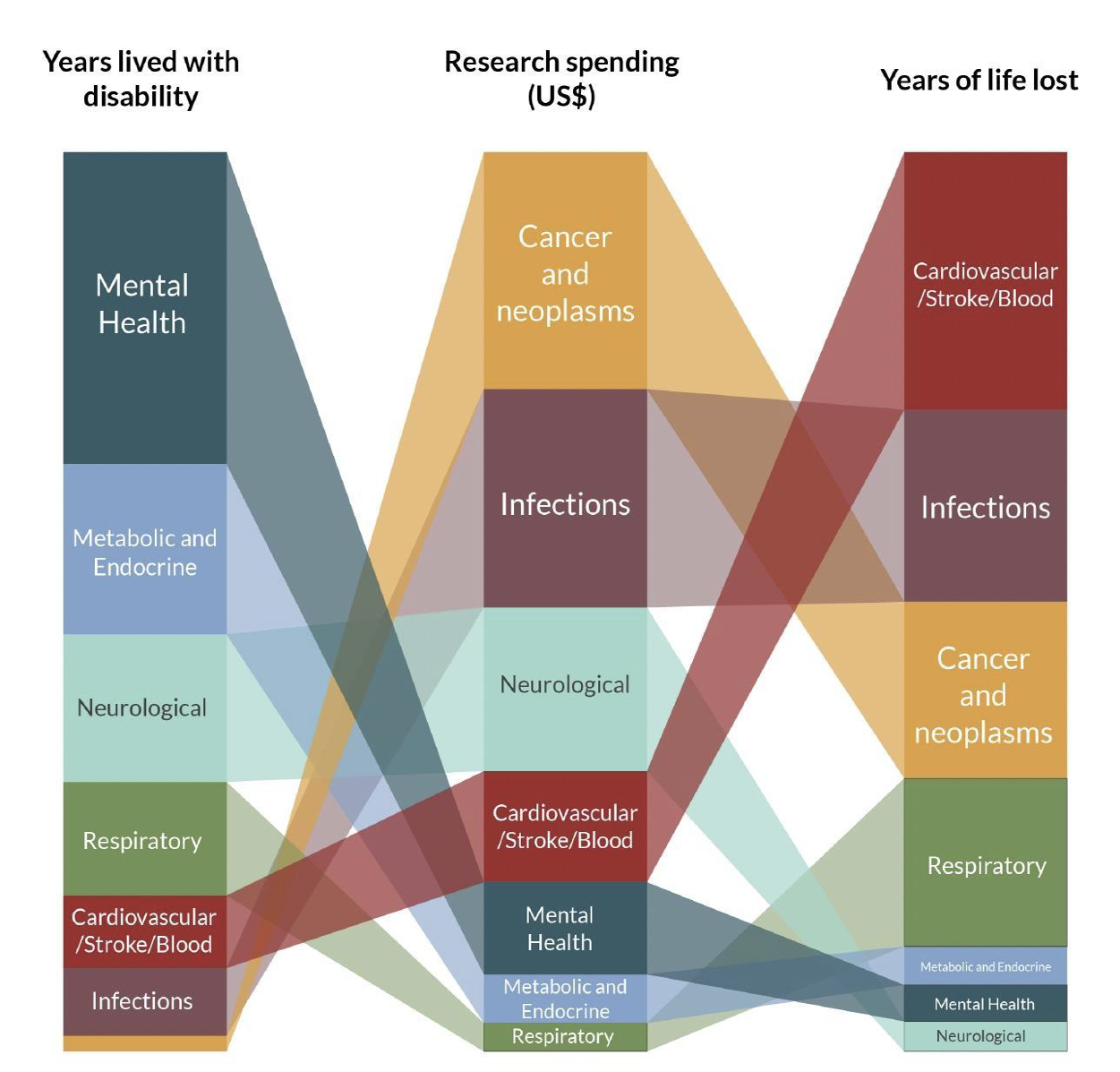
For example, while cancer research received US$755 for every YLD(year lived with disability), mental health research received only US$15. Note that since cancer causes more years of life to be lost than mental health, some difference should be expected. But a difference of 50x is disproportionate. (I have been unable to find the raw data behind this figure to get a precise estimate of what difference we should expect. Eyeballing the figure below, we can see that neurological disease causes roughly half the number of YLD and fewer YLL than mental health, but receives twice as much funding. So an increase of at least 3x in mental health funding would be needed to “balance” out this difference.)
Figure 3: Burden of disease for selected health research categories, compared to amount spent on research
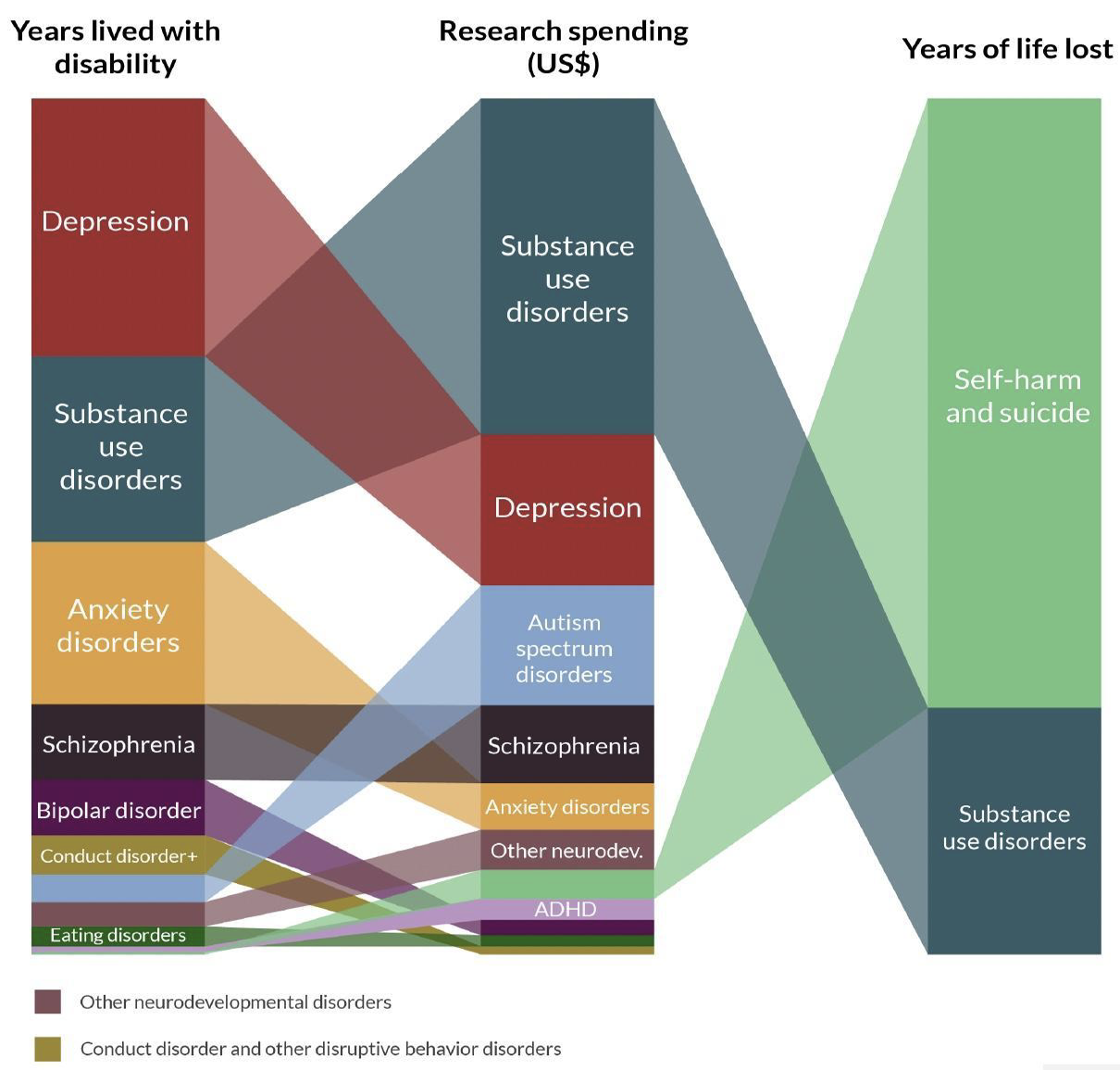
Suicide and self-harm are underfunded compared to other areas of mental health.
Despite causing over half of years of life lost to mental illness, they received only 4.3% of mental health research funding.
Figure 4: Burden of disease for selected conditions compared to amount spent on research
Underfunding is a particular issue in developing countries, which account for 77% of global suicides.
Health expenditure per person is disproportionately low in developing countries. In the chart below, we see an overall positive relationship between wealth and health expenditure. But the trend is not linear. Among poorer countries, the trend is steeper: a given increase in health expenditure requires a greater increase in GDP per capita than among rich countries.[4]
Figure 5: Health Expenditure per capita versus GDP per capita
There are also fewer psychiatrists working in mental health in developing countries. For example, Togo has only two psychiatrists working in mental health in a population of 8.3 million people. The chart below shows that psychiatrist density is disproportionately low in developing countries. Among poor countries, a given increase in wealth is associated with a smaller increase in the number of psychiatrists than among rich countries.[5]
Figure 6: Psychiatrists working in mental health per 100,000 versus GDP per capita
From the above data on mental health funding, healthcare funding, and psychiatrists working in mental health, we can reasonably believe that mental health work is neglected globally and particularly in developing countries.
If we are comfortable with the idea that a large part of suicide prevention will involve work in mental health, then it seems reasonable to conclude that a large part of suicide prevention is underfunded and neglected.
Beyond the quantitative evidence
But it is also worth considering qualitative arguments for why suicide prevention might be globally neglected. As discussed, there is no easily available data on funding and work on suicide prevention in general. When data is missing or biased, it is useful to consider the qualitative as well as the quantitative. And there are strong reasons to believe that suicide prevention is neglected.
In the rich western world, mental health has become a more common, less taboo topic, thanks to the work of many charities and campaigning organisations. I live in the UK, where anxiety and depression are talked about reasonably openly. More serious mental health conditions like bipolar disorder and schizophrenia are still relatively undiscussed. Suicide and self-harm are even more sensitive and sometimes taboo topics, only to be brought up among close friends or family. For example, I’ve found myself lowering my voice when discussing this essay. Even in parts of the world where we are actively trying to be more open about mental health, suicide remains a taboo. It seems reasonable to believe therefore that in parts of the world where mental health issues in general are still shameful, let alone in those where suicide is a criminal offence, suicide will be discussed even less. This hypothesis would benefit from some testing, for example by interviewing mental health experts in different parts of the world.
In parts of the world where suicide is criminal, or even just stigmatised, we should expect that the extent of suicidal ideation is hidden as sufferers are unlikely to come forward for help. This means that the demand for suicide prevention is hidden. When any problem is under-highlighted, we should expect insufficient funding and a lack of talented people working to solve it, resulting in the problem not being solved as efficiently as it could be. It seems unlikely that suicide would be different. So, we should expect that the criminalisation and stigmatisation of suicide leads us to neglect suicide prevention.
Landscape
Who else is working on this?
I haven’t been able to find anyone working on suicide prevention beyond mental health work. The evidence on divorce policy reducing suicide rates (see below) makes me optimistic that there may be areas of work that are completely neglected and therefore where Open Philanthropy could make a big difference. The first step would be to scope areas where suicide rates may be improved by interventions, both looking at existing research and potentially funding studies in this area.
There are however many groups working in suicide prevention via mental health. I take most of the data below from a 2016 ODI report.
Country governments are the primary funders of mental health work.
Of the 171 countries that contribute to the WHO 2014 Mental Health Atlas, 71% stated that their national budget was the primary source of funding for mental health, and 18% listed households as the primary source of funding.
Despite this, they often spend less than 1% of national health budgets on mental health specifically. Most poorer countries also spend most of this on mental hospitals, which is inefficient compared to community-based services. Even worse, 30% of the 184 countries surveyed for WHO’s 2005 Mental Health Atlas did not have a specified mental health budget. I have been unable to find a more up-to-date figure on this.
This shortfall often means that households must bear the costs.
While the total economic burden on households is yet to be established, there have been efforts to calculate these figures. One of the few studies available found that 15% of women with a common mental disorder in India spent more than 10% of household income on health-related expenditures (Patel et al., 2006). These are often the households that are least able to afford such a cost.
Development assistance has slowly increased but remains insufficient. In a study published in 2015, Gilbert et al. found that, although funding had tripled, it still accounted for less than 1% of total health spending. Mental health funding has therefore increased at a slower rate than other kinds of health spending.
The top three donors giving development assistance to mental health are the WHO, European Union (EU) Institutions and the United States. The WHO aid is also limited by its mandate to provide technical advice rather than fund services on the ground.
More funding is needed.
The Lancet Global Mental Health Group estimated the minimum needs to be scaling up a basic mental health care package to US$2 per capita per year in low-income countries (Lancet, 2007). In 2011, the WHO Mental Health Atlas estimated mental health expenditure in low-income countries to be US$0.20 per capita, with donor assistance (recorded with the DAC Creditor Reporting System) adding a further US$0.05 per capita (Gilbert et al., 2015: 3). This means that only 25 cents per capita is spent, compared to the US$2.00 per capita that is needed to meet basic mental health care costs. To meet this minimum needed, as asserted by global experts, we need to find a remaining $1.75 per person.
Tractability
How might we go about trying to reduce suicide rates?
There are some established avenues in effectively reducing suicides. Beyond these, more research is needed into effective methods. Open Philanthropy could help both by funding research and pilot studies to broaden the evidence base on effective suicide prevention. But it could also help to scale interventions that have already been shown to be effective.
Lobbying for unilateral divorce wherever it is not yet legal may decrease suicide rates among married women. The mechanism here might be that by giving women the option to divorce their husbands, they gain bargaining power within their marriage, reducing abuse and violence. (Interestingly, divorce rates didn’t increase much, suggesting this effect was not driven by women actually leaving their marriages.) If your partner knows you can leave them if they go too far, they are less likely to do so. This was shown by Stevenson and Wolfers (2006), who exploited variation from different timing of divorce law reforms across the US to show that enactments of unilateral divorce led to reductions in suicide rates, mainly for women aged 25-65. Overall, they find that total female suicide fell by around 20% in the long run in states that adopted unilateral divorce. Their findings in terms of increase bargaining power are echoed by Brassiolo (2016), who finds a decrease in spousal violence as a consequence of divorce law reform in Spain. Context does seem to matter for this effect, however, as Hoehn-Velasco and Silverio-Murillo (2020) find no effect of divorce law reform on female suicide and homicide in Mexico. The authors conclude that women in Mexico are unable to escape their abusive marriages through divorce, despite the legal changes.
The research above positions lobbying for unilateral divorce as a potentially effective lever in reducing suicide rates. Before funding such lobbying, we should first conduct further research to either strengthen or reject the hypothesis that divorce law does reduce suicides, and to investigate the role of country context. For example, if we think the zero-effect in Mexico was due to a weak rule of law, we could ideally test this hypothesis by conducting similar research to the above papers using data in countries with varying legal strength.
If we were satisfied that unilateral divorce policy is an effective mechanism to reduce suicide rates, the effect could be dramatic. Given that 246,015 women kill themselves every year, successfully lobbying for unilateral divorce legalisation across the world could prevent 49,203 annual suicides. This is an overestimate of the potential effect as in many countries unilateral divorce is already legal. Successfully lobbying for this change in a single country of 40 million people, where 1,260 women kill themselves each year, could save around 252 women’s lives saved annually.[6] A precise estimate of the potential global impact would require research into the number of countries where unilateral divorce is illegal.
Effectively reducing alcohol abuse may reduce suicide rates. Alcohol use is strongly associated with suicide. Those with alcohol addiction are 120 times more likely to commit suicide. It is difficult (within the constraints of medical ethics) to prove a causal link between alcohol abuse and suicide. But we can use reasoning, alongside the empirical association between them, to establish that there is probably a causal effect. Of course, many people in serious distress use alcohol to self-medicate to cope with their problems. If the problems, and self-medication, are chronic, this could develop into a dependence and perhaps even an addiction. So there is reason to believe that some of this associative effect may be due to those being prone to suicide anyway, also being prone to alcoholism. But there is strong reason to believe that while alcohol addiction will increase the risk of suicide for anybody, this effect will be particularly strong for those with mental health disorders, or who are already in extreme distress. Alcohol addiction can cause even greater strain on one’s relationships, jobs, body and mind than the underlying stressors which caused us to turn to alcohol. Alcohol also exacerbates the symptoms of mental health conditions like bipolar disorder, borderline personality disorder, and depression, all of which contribute to suicide. In the mid-to-long-term, alcohol abuse makes suicidal ideation both more frequent and intense, increasing the risk of suicide. A causal link between alcohol abuse and suicide seems highly likely.
There is substantial evidence that alcohol taxation, as well as restricting the availability of alcohol (e.g. through age and time constraints to purchasing it), lead to reduced consumption and a fall in alcohol-related social problems, including suicide. I refer you both to Ősterberg E. (2004) and to Open Philanthropy’s own work in this area, for example David Roodman’s review of the evidence on taxation.
There is a very strong link between mental health disorders and suicide. Two broad ways we can reduce suicide is by (a) implementing and expanding existing treatments for mental health disorders, and (b) funding further research into those mental health conditions strongly linked to suicide. The former will likely be focussed in developing countries where the access to psychosocial support and medications is limited. The latter would most likely be focussed on research institutions.
All the above methods will likely improve the lives of people above the critical threshold of happiness discussed above, and not just those with suicidal thoughts.
Who or what would I fund?
There are two types of projects Open Phil could fund to effectively reduce suicide rates. My first grouping includes projects that have an existing evidence base behind them, and require funding to scale the intervention or introduce it in new places.
Under this I would include, for example:
funding lobbying for unilateral divorce policy in countries where it is not yet legal
funding alcohol taxation/control lobbying, focussing on countries where the alcohol abuse rate is high, and there is a strong association with suicides
funding training for community-based psychosocial support workers in developing countries
A second grouping of projects aims for incredible results but requires more upfront investment. These projects are the “venture-capital-style” philanthropy projects.
Under this I would include, for example:
funding research into treatment/cures for mental health disorders strongly associated with suicide, like schizophrenia
funding research into policy interventions that could improve suicide rates, in the style of Stevenson and Wolfers—this might take the form of funding economics PhD research into this area, or research groups focussed on effective policy.
Further Questions
Concerns about specific interventions
As discussed above, the intervention to reduce female suicides by lobbying for unilateral divorce laws depends on the effect being similar to that seen in the papers looking at the US and Spain, and not the zero-effect seen in Mexico. See my discussion under “Tractability” for details of next steps to strengthen or reject this hypothesis.
The interventions which would expand access to the kind of mental health support we have in the rich world, depend on the assumption that mental health provision in the rich world works. One unresolved worry I have is that the geographic distribution of suicide rates looks reasonably similar between developing and developed countries.
We could infer from this that all the resources spent by rich countries are not terribly effective. This contrasts with the WHO recommendations on cost-effective mental health provision, but I have been unable to find the evidence behind the WHO’s stances that community based psychosocial support workers are effective.
One reason to doubt this conclusion that rich country resources are not well spent might be that the suicide underreporting bias is greater in poorer countries, so while the measured rates might be similar, the true underlying rates might be different. In order to answer this question we would need a greater understanding of the scale of underreporting in different countries.
If we cannot find a good reason behind the WHO’s stance on community-based psychosocial report, and we do find that estimates of suicide rates in rich and poor countries are likely biased to a similar extent, then we shouldn’t pour money into funding these ineffective interventions in developing countries. Instead, it may end up being more cost effective to direct our money into frontier mental health research, to try and find effective ways of dealing with serious mental health issues and prevent suicide. Let’s not waste money scaling up ineffective solutions.
Estimating the dollar impact of interventions
With more time and resources, the next step would be to cost out the dollar impact of different types of interventions to prevent suicide. I think the best way to measure impact would be to look at suicides prevented per dollar. As discussed above, this would be an underestimate of the full impact of the intervention, as we will have multiplier effects via loved ones not being harmed by suicide, and the lives of people in the rest of the distribution being improved. I am not sure there is an obvious reasonable method with which to come up with this multiplier. One reasonable response to this data issue could be to leave out the multiplier and accept that all impact estimates will be underestimates.
Below, I have provided a framework of questions to answer to get this estimate for the evidence-backed interventions I have proposed. As some questions get answered, no doubt more will be added to the list. Some of the below questions will likely require speaking to an expert. For the more uncertain, long-term, “venture-capital-style” interventions, I would imagine we would need to use a venture-capital-style to model both probability of success and impact if successful. This would require further time and research to do properly.
To estimate the per dollar impact of lobbying for unilateral divorce:
Which countries currently lack unilateral divorce?
What would the likely dollar-cost of lobbying for this successfully be in each of these countries?
Then,
(Annual female suicides in country A x 20%) / Dollar cost of lobbying
would give the number of suicides prevented annually over dollar cost. We could then have a list of the most effective countries to work in, in impact per dollar terms.
To estimate the per dollar impact of alcohol control policy:
Which countries have the worst alcohol abuse and/or alcohol-abuse linked suicide rate?
What is the estimated impact of a x% tax increase on alcohol abuse?
What would the likely dollar-cost of lobbying for this successfully be in each of these countries?
What is the estimated impact of a ban on alcohol purchasing at certain times on alcohol abuse?
What would the likely dollar-cost of lobbying for this successfully be in each of these countries?
What share of a reduction in alcohol abuse will feed through into alcohol-linked suicides?
Then,
(Reduction in alcohol abuse x Share of reduction that feeds through to alcohol abuse linked suicide) / Dollar cost of lobbying for legal change
would give the number of suicides prevented annually over dollar cost. We could then compare tax and other forms of alcohol control, and have a list of the most effective countries to work in, in impact per dollar terms.
To estimate the per dollar impact of training psychosocial support workers in developing countries:
How much does it cost to train a community psychosocial support worker in country/region X?
How does access to a psychosocial support worker impact suicide rates?
What are suicide rates in country/region X?
Then,
(Suicide rate x expected reduction in suicide rate from access to a psychosocial support worker) / cost of training
would give the number of suicides prevented annually over dollar cost. We could then compare regions in terms of most effective areas to work in.
- ^
This is likely to be an underestimate due to many suicides being officially categorised as accidents due to social and religious attitudes, and in some cases the illegality of suicide.
- ^
This is an imprecise estimate that would benefit from a more thorough investigation. There are 25 suicide attempts for every suicide in the US (WMICH). I have been unable to find data on the number of individuals who attempt suicide for every person that succeeds. Since 16.3% of suicide attempters go on to re-attempt, the number of attempts will overestimate the number of individuals. I have also been unable to find data on the average number of suicide attempts. Assuming that those who re-attempt suicide, re-attempt an average of once, we should expect around 21 suicide-attempters for every successful suicide. (I have been unable to find global figures, but national figures seem like a reasonable baseline for a back-of-the-envelope calculation.) A clear next step here would be to find more precise figures on the number of attempters for every successful suicide.
- ^
This argument should apply whatever the shape of the distribution, but it’s easier to intuit the diagram if we draw it as normal.
- ^
I have excluded countries with GDP per capita above 60k in the chart below to better see the distribution of poorer countries. This excludes Qatar, Luxembourg, Singapore, Kuwait, the UAE and Norway from the visible sample.
- ^
I have again excluded countries with GDP per capita above 60k in the chart below to better see the distribution of poorer countries. This excludes Qatar, Luxembourg, Singapore, Kuwait, the UAE and Norway from the visible sample.
- ^
These calculations uses the 2017 female suicide rate of 6.3, taken from https://ourworldindata.org/suicide, as well as Stevenson and Wolfer’s estimated effect size of a 20% reduction in female suicide
I think you’re definitely right that suicide prevention is a crucial and underfunded public health issue. I think, however, that this post could use some more input from empirical work on suicidology.
You express some doubt about approaches that reduce access to means, because these merely “delay the irreversible action . . . it does not fix the issue we care about—people not valuing their own lives.”
I am skeptical about this. Consider: “Between 1963 and 1975 the annual number of suicides in England and Wales showed a sudden, unexpected decline from 5,714 to 3,693 at a time when suicide continued to increase in most other European countries. This appears to be the result of the progressive removal of carbon monoxide from the public gas supply.” (Clarke and Mayhew, 1988) Note that these potential suicides were not displaced to other means, or delayed—they simply never happened at all. The low-hanging fruit in suicide prevention are similar interventions on means, in country-specific ways: gun control in the United States, pesticides in large parts of rural China, etc.
One might respond that these interventions don’t really touch the fundamental issue, which is whether people value their own lives or not. I’m inclined to argue the other way around: the fact that suicide rates shift so profoundly in response to availability of means suggest that they are not a good proxy for the value people place on their own lives. When we are concerned with the value people place on their own lives, we are most concerned with their stable and reflective judgments, and it is doubtful that suicide is revelatory of these.
One book that I found extremely helpful on summarizing and extending our best understanding of the psychology of suicide is Thomas Joiner, _Why People Die By Suicide_.
Immediate thought here was that suicidal ideation is comorbid with depression and that there’s some evidence that psychotherapy seems to be cost-effective: https://www.happierlivesinstitute.org/report/psychotherapy-cost-effectiveness-analysis/