Why are we not using upper-room ultraviolet germicidal irradiation (UVGI) more?
| This is a Draft Amnesty Week draft. It may not be polished, up to my usual standards, fully thought through, or fully fact-checked. |
Commenting and feedback guidelines:
|
Please be aware that I wrote all of this in November 2022 and haven’t engaged with the draft since. I have learnt much more about germicidal ultraviolet since and probably don’t agree with some of the takes here anymore. I am posting it to get it out there instead of having it lying around in some Google doc forever.
I am currently operating under the hypothesis that upper-room UVGI systems are efficacious, safe, and cost-effective for reducing the transmission of airborne diseases (E. A. Nardell 2021; E. Nardell et al. 2008; Abboushi et al. 2022; Shen et al. 2021). We have known about them since the 1940s. I was interested in digging into the history of research on upper-room UVGI to answer the question: If we have known for so long how well upper-room UVGI works, why are we not using it much more widely?
Summary
The points below are largely bad reasons not to use upper-room UVGI, which leads me to suspect that upper-room UVGI is underrated and that we should probably be implementing it more.
Upper-room UVGI is an 80-year-old technology.
The first epidemiological studies in the 1940s were very promising but attempts to replicate them were much less successful.
The studies which did not show an effect likely had important design flaws.
Around the same time that the epidemiological studies showing limited effects were published, other measures for combating tuberculosis were invented. Thus, upper-room UVGI became less of a priority.
People were concerned about the safety of UVC light. These concerns are mostly unjustified today, but many people are still worried and extremely reluctant to implement upper-room UVGI.
While some guidelines exist, there are no government standards for upper-room UVGI. The regulatory environment in the US is a mess, leaving manufacturers and consumers with a difficult market.
The medical establishment has been overly skeptical of airborne disease transmission in the 20th century and partly until today. Technologies for combating airborne disease transmission were therefore overlooked.
Early epidemiological studies
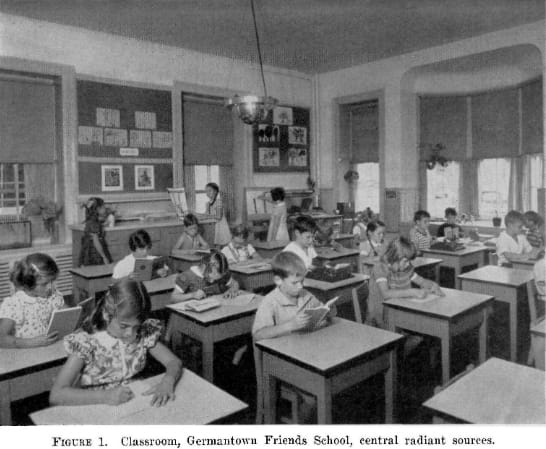
Initial studies on the effectiveness of upper-room UVGI and UVGI “light barriers” in the 1940s showed great promise (Sauer, Minsk, and Rosenstern 1942; Wells, Wells, and Wilder 1942). For instance, in the Wells trial during the 1941 Pennsylvania measles epidemic, 60% fewer susceptible children were infected in the classrooms with upper-room UVGI (see Appendix 2 for an extensive spreadsheet).
These promising results prompted further epidemiological studies in the 1940s and 50s, but those did not show a significant effect, and people felt disillusioned with the technology (Reed 2010).
Kowalski, one of the leaders in modern UVGI research, claims that the MRC study (1954) played an essential role in the declining interest in upper-room UVGI (Kowalski 2009, 11). That study concluded: “There was no appreciable effect on the total sickness absence recorded in either the Infant or the Junior departments. [...] The effect of irradiation on total sickness absence is therefore small, and the results would not appear to justify wide use of irradiation as a hygienic measure for the control of infection in primary urban day schools.” (Medical Research Council (Great Britain) 1954).
One problem with the study was that while upper-room UVGI was installed in the classrooms, the students shared other indoor environments where they could become infected (Jimenez et al. 2022; Reed 2010; E. Nardell, Vincent, and Sliney 2013). To illustrate this: The children who sat together in the irradiated classroom might have also ridden on the same school bus, where no upper-room UVGI system was installed. Thus, they had ample opportunity to infect each other, and comparing days of absence of kids in the irradiated classrooms with those in the control classrooms did not show a meaningful effect. This is a key issue that makes it hard to run good epidemiological studies on air disinfection.
Tuberculosis
Here is a quote from the Centers for Disease Control and Prevention (CDC): “Since 1950, the bulk of the research on upper-room UVGI systems focused on controlling the spread of tuberculosis (TB).” The CDC’s most up-to-date guidance on implementing upper-room UVGI systems is also focused explicitly on controlling tuberculosis (NIOSH 2009). Until today, TB is the infectious disease that causes the most deaths worldwide. Thus, interest in upper-room UVGI during the 1940s and 1950s was, presumably, also focused on TB. Around the same time that the lacking epidemiological studies about upper-room UVGI were published, scientists made key discoveries to combat TB, so they became relatively less interested in the potential of UVGI (Riley and Nardell 1989). Albert Schatz discovered streptomycin in 1943, the first antibiotic treatment against tuberculosis (W. Kingston 2004). In the 1950s, many governments started using the BCG vaccine against TB. The UK, for example, introduced it into its vaccine schedule in 1953.
With falling TB infections in developed countries like the US—where the research on upper-room UVGI took place—people became relatively less interested in upper-room UVGI for decreasing the risk of infection.
Concerns about the safety of UVGI:
People in the 1950s likely also stopped paying attention to UVGI because they had some concerns about the technology that were valid at the time (Riley and Nardell 1989). Only a few of these are still relevant today, and I address them in Appendix 3. From Reed (2010): “Additionally, there was concern regarding the health effects from UV-C exposure and the production of ozone by germicidal lamps. Concerns that UVGI required high maintenance, that UVGI would be ineffective at higher humidity, and that its germicidal efficacy was unproven also contributed to UVGI’s second-class status among air disinfection strategies.”
Lack of standards on UV air disinfection
This section was largely informed by talking to Ernest Blatchley. He claims that the lack of standards plays a key role in the limited uptake that upper-room UVGI has seen, and I find this very plausible.
While the National Institute for Occupational Safety and Health (NIOSH) gives some guidelines, no clear government standards exist for upper-room UVGI or indoor air quality. This results in a lack of quality control and unclarity around the treatment objective of upper-room UVGI air disinfection. Compare this to the treatment of drinking water. Government agencies—e.g. the EPA in the US—set legally enforced limits for the tolerable amount of dozens of different contaminants in drinking water. Furthermore, they specify how often and with which methods drinking water must be tested for these contaminant levels. Most importantly, these legal limits are adjusted to the risk of disease. The association between certain levels of contaminants and resulting health risks are clearly understood. The standards are similar in other developed countries, so you can drink tap water without giving much thought to whether that is safe.
The regulatory environment for UVGI is a wild west. If it is a medical product, it falls under the mandate of the Food and Drug Administration (FDA). Since UV light can kill microbes, it is a pesticide in the broadest sense, which means it is regulated by the Environmental Protection Agency (EPA). Then there are the CDC and NIOSH, which make recommendations for the use of upper-room UVGI to inhibit disease transmission. Overall, it is very complicated, and the responsibilities seem unclear.
While there are no standards from the government, UVGI manufacturers can get a certification for their products from UL Solutions, a for-profit company.
In practice, this unclear regulatory situation results in a UVGI market where some products are questionable, ineffective, or dangerous for consumers. These dubious products harm the legitimacy of other UV technologies, such as upper-room UVGI (E. A. Nardell 2021).
A lack of standards probably inhibits the uptake of upper-room UVGI for air disinfection because
there are no incentives for companies to install it. It would be more widespread if upper-room UVGI were included in standards for indoor air quality and building codes and thus mandatory to install.
consumers face a market where it is hard to understand which products are legitimate. This results in little demand and fewer manufacturers selling UVGI products.
General skepticism of airborne transmission by the medical establishment
From ~1920 until the 1980s (and partly until today), the medical establishment was very skeptical of airborne transmission—a kind of systematic overreaction to the earlier false belief in miasma theory (Jimenez et al. 2022). If you think that airborne transmission does not exist, you will not focus on interventions that reduce indoor airborne transmission, such as upper-room UVGI.
An uncharitable interpretation here is that public health experts might have been subject to subconscious motivated reasoning along the lines of, “If airborne transmission exists, then we cannot simply tell doctors to wash their hands to reduce transmission but would need to retrofit buildings with upper-room UVGI, and that is annoying and expensive.” If this was the case, many scientists had the incentive to remain skeptical of airborne transmission in general.
Upper-room UVGI has a PR problem.
Many people perceive upper-room UVGI as more dangerous than it is. They associate “UV” with being unsafe and causing cancer. The word radiation sounds even scarier, and most humans are generally very risk-averse. While upper-room UVGI is remarkably safe if implemented correctly, a small risk of exposure and the resulting harm cannot be ruled out (E. Nardell et al. 2008). From my impression of talking to people who have tried to popularize the use of upper-room UVGI, it is very tough to convince people of its safety. If even the slightest risk of harm exists, people will be reluctant to use the technology. Thus, I imagine decision makers who would be responsible for buying and installing upper-room UVGI in, e.g., hospitals, prefer other systems with no risk, like air purifiers, even when they are less (cost-)effective.
Conclusion
In my impression, history could have easily turned out otherwise. It seems like a historical accident that disappointing epidemiological studies on upper-room UVGI appeared around the same time as other solutions to tuberculosis. When combining this with concerns about the safety of UVGI, a lack of standards, and systematic skepticism of the medical establishment around airborne transmission, it becomes clear why upper-room UVGI systems are not widely used.
These are largely bad reasons not to use upper-room UVGI, which leads me to suspect that upper-room UVGI is underrated and that we should probably be implementing it more.
More speculative reasons that I do not have clear evidence for
people do not want to pay upfront costs for hypothetical future payoff and are therefore not super interested in installing upper-room UVGI to prevent infections
especially when it is unclear how large the benefit is in any given year
if there is a pandemic, then the benefit is large but otherwise not as much
basically getting people to care much about prevention is hard
My guess is that a few very dedicated people like Wells and Riley pushed the frontier of research on upper-room UVGI forward. When they retired, there were very few researchers interested in continuing their work.
AFAICT, Wells alone is responsible for something like a third of all the upper-room UVGI epi studies.
These PubMed charts of publication dates on different keyword searches could give a rough approximation of interest over time:
the 40s and 50s (?) were also the time when important standards were set for indoor air quality in building regulations and stuff, and because this was exactly the time when upper-room UVGI fell out of favor due to the lacking studies, it wasn’t included in those new standards
Appendix 1: Key quotes from sources that Reed (2010) cites as “other failures” that led to disillusionment with upper-room UVGI.
“The incidence of air-borne diseases, as judged by hospital admission records, in nonirradiated and irradiated dormitories showed no significant difference under the conditions of this experiment. The variation among the dormitories was so great that no statement can be made concerning the influence of ultraviolet light upon the incidence of air-borne infection insofar as these experiments are concerned.” (Schneiter et al. 1944)
“The disease incidence among the inhabitants of the radiated dormitories was sometimes higher, sometimes lower, than that of the control dormitories, with no evidence that ultraviolet radiation consistently effected a reduction in disease incidence. 5. Since no significant effect of ultraviolet in controlling disease incidence could be detected among a population of about 400 inmates during 6 years, the beneficial effect of ultraviolet installations for general population use is questioned.” (Dubuy et al. 1948)
“These analyses of epidemics of mumps in two of the centralized schools under study offer no incontrovertible evidence that ultra-violet lamps in the classrooms modified the spread of the disease in those classrooms. This finding may indicate that ultra-violet irradiation is ineffective in controlling the spread of mumps, or it may mean merely, as some authorities believe, that mumps is not an air-borne infection.” (Bahlke, Silverman, and Ingraham 1949)
“Mechanical ventilation at 7 air changes/hr., air disinfection using vaporized hexyl resorcinol or ac-hydroxy-oc-methyl butyric acid, or irradiation of the air of the room above 8 ft. with ultraviolet radiation when applied to various clerical offices did not result in any observed alteration in the numbers of colds experienced by those working in them.” (D. Kingston, Lidwell, and Williams 1962)
Appendix 2: Epidemiological studies I found on upper-room UVGI
Table from (Kowalski 2009, 226):
I recreated the table in a spreadsheet to add studies that he did not include and more columns with further useful information: Field trials and other efficacy studies of upper-room UVGI
I also think there are at least a few mistakes in Kowalski’s table so I wouldn’t take it at face value.
I calculated the number of 60% fewer infections in classrooms with upper-room UVGI myself by using the data given in (Wells, Wells, and Wilder 1942). 59% of children became infected in unirradiated classrooms, and 24% of children became infected in irradiated classrooms The calculation can be found in the fields E4 and F4 of the spreadsheet.
Appendix 3: Addressing safety concerns about upper-room UVGI
Exposure to 254 nm UVC light can indeed lead to temporary impairment like skin erythema and eye damage (NIOSH 2009, 5; Kowalski 2009, 287). For this reason, upper-room UVGI systems must be implemented with safety in mind. Emphasis should be put on correct installation by professional technicians, and the UV fixtures need to include louvers that prevent any direct irradiation from reaching people in the lower room.
Ozone generation only becomes relevant with UVC wavelengths lower than 240 nm (Kowalski 2009, 307). Upper-room UVGI systems that use conventional filtered Hg LP lamps with a peak at 254 nm do not have an issue with significant ozone production (Bahnfleth 2021).
Relative humidity (RH) affects UV rate constants (UV susceptibility), but these effects are small in the contexts where upper-room UVGI is implemented. UV rate constants tell you how much dose is needed to kill a certain pathogen. The lower the UV rate constant, the larger the dose needed to inactivate the pathogen.
Relative humidity in a typical workplace environment is usually between 40% and 60%. From (Kowalski 2009, 75), explaining the table below: “The term “Lo RH” refers to relative humidity below about 68% while “Hi RH” implies an RH of about 68% or higher.” Thus, relative humidity effects on UV rate constants only become relevant at levels significantly higher than what is typically the case in environments where upper-room UVGI is implemented. Furthermore, relative humidity effects on UV rate constants are largely insignificant for viruses, which is the microbial group we are most interested in combating when it comes to really scary pandemics.
Appendix 4: A few notes on UV water disinfection and its relation to UV air disinfection
UV started to be used much earlier for water than for air disinfection (Kowalski 2009, 3)
1909 First European applications for UV water disinfection
1936 First overhead UV system in hospitals
UV water disinfection is a much bigger commercial market than UV air disinfection
The global ultraviolet disinfection equipment market size is projected to surpass US$ 5.7 billion by 2027 from estimated US$ 2.5 billion in 2019. [...] In 2019, the use of UV disinfection equipment in applications for water & wastewater treatment led the industry and accounted for 70.4% of global sales.
the global UV disinfection equipment market is expected to grow from USD 5.6 billion in 2021 to USD 20.01 billion by 2030. [...] In 2021, the water and wastewater treatment segment dominated the market, with the largest market share of 31% and market revenue of 1.7 billion.
The global UV disinfection equipment market was valued at US$ 3.07 Bn in 2020. [...] As of 2020, the water treatment segment held a share of 56.5% of the global UV disinfection equipment market.
The scientific field of UV water disinfection is much more developed than the field of UV air disinfection
Blatchley said “The field of UV air disinfection is currently at the point where UV water disinfection was roughly 30 years ago”
Bibliography
Abboushi, Belal, Gabe Arnold, Jason Tuenge, and Tim Salsbury. 2022. “Energy Implications of Using Upper Room Germicidal Ultraviolet Radiation and HVAC Strategies to Combat SARS-CoV-2,” 16.
Bahlke, Anne M., Hilda Freeman Silverman, and Hollis S. Ingraham. 1949. “Effect of Ultra-Violet Irradiation of Classrooms on Spread of Mumps and Chickenpox in Large Rural Central Schools —A Progress Report.” American Journal of Public Health and the Nations Health 39 (10): 1321–30.
Bahnfleth, William P. 2021. “Ultraviolet Germicidal Irradiation (UVGI) Can Be Used in Conjunction with HVAC Systems or in Spaces to Disinfect Air and Surfaces to Reduce Disease Transmission, Control Biofouling of Cooling Coils in Air-Handling Units and Improve Indoor Air Qual- Ity (IAQ). The Use of This Technology Escalated amid the COVID-19 Pandemic, Leading to Increased Questions and Misconceptions.,” February, 2.
Dubuy, H. G., J. E. Dunn, F. S. Brackett, W. C. Dreessen, P. A. Neal, and I. Posner. 1948. “AN EVALUATION OF ULTRAVIOLET RADIATION OF SLEEPING QUARTERS AS SUPPLEMENT OF ACCEPTED METHODS OF DISEASE CONTROL1.” American Journal of Epidemiology 48 (2): 207–26. https://doi.org/10.1093/oxfordjournals.aje.a119236.
Jimenez, Jose L., Linsey C. Marr, Katherine Randall, Edward Thomas Ewing, Zeynep Tufekci, Trish Greenhalgh, Raymond Tellier, et al. 2022. “What Were the Historical Reasons for the Resistance to Recognizing Airborne Transmission during the COVID-19 Pandemic?” Indoor Air 32 (8): e13070. https://doi.org/10.1111/ina.13070.
Kingston, D., O. M. Lidwell, and R. E. O. Williams. 1962. “The Epidemiology of the Common Cold.” The Journal of Hygiene 60 (3): 341–52.
Kingston, William. 2004. “Streptomycin, Schatz v. Waksman, and the Balance of Credit for Discovery.” Journal of the History of Medicine and Allied Sciences 59 (3): 441–62. https://doi.org/10.1093/jhmas/jrh091.
Kowalski, Wladyslaw. 2009. Ultraviolet Germicidal Irradiation Handbook: UVGI for Air and Surface Disinfection. Berlin, Heidelberg: Springer Berlin Heidelberg. https://doi.org/10.1007/978-3-642-01999-9.
Medical Research Council (Great Britain). 1954. Air Disinfection with Ultra-Violet Irradiation; Its Effect on Illness among School-Children. Medical Research Council [Great Britain]. Special Report Series,No. 283. London: H. M. Stationery Off. https://catalog.hathitrust.org/Record/001682089.
Nardell, Edward A. 2021. “Air Disinfection for Airborne Infection Control with a Focus on COVID-19: Why Germicidal UV Is Essential†.” Photochemistry and Photobiology 97 (3): 493–97. https://doi.org/10.1111/php.13421.
Nardell, Edward, Scott Bucher, Philip Brickner, Charles Wang, Richard Vincent, Kathleen Becan-McBride, Mark James, Max Michael, and James Wright. 2008. “Safety of Upper-Room Ultraviolet Germicidal Air Disinfection for Room Occupants: Results from the Tuberculosis Ultraviolet Shelter Study.” Public Health Reports (Washington, D.C. : 1974) 123 (January): 52–60. https://doi.org/10.1177/003335490812300108.
Nardell, Edward, Richard Vincent, and David H. Sliney. 2013. “Upper-Room Ultraviolet Germicidal Irradiation (UVGI) for Air Disinfection: A Symposium in Print.” Photochemistry and Photobiology 89 (4): 764–69. https://doi.org/10.1111/php.12098.
NIOSH. 2009. “Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation Guidelines for Healthcare Settings.” U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. https://doi.org/10.26616/NIOSHPUB2009105.
Reed, Nicholas G. 2010. “The History of Ultraviolet Germicidal Irradiation for Air Disinfection.” Public Health Reports 125 (1): 15–27. https://doi.org/10.1177/003335491012500105.
Riley, Richard L., and Edward A. Nardell. 1989. “Clearing the Air: The Theory and Application of Ultraviolet Air Disinfection.” American Review of Respiratory Disease 139 (5): 1286–94. https://doi.org/10.1164/ajrccm/139.5.1286.
Sauer, L. W., L. D. Minsk, and I. Rosenstern. 1942. “CONTROL OF CROSS INFECTIONS OF THE RESPIRATORY TRACT: IN A NURSERY FOR YOUNG INFANTS: A PRELIMINARY REPORT.” Journal of the American Medical Association 118 (15): 1271. https://doi.org/10.1001/jama.1942.02830150007003.
Schneiter, R., A. Hollaender, B. H. Caminita, R. W. Kolb, H. F. Fraser, H. G. Du Buy, P. A. Neal, and H. B. Rosenblum. 1944. “EFFECTIVENESS OF ULTRAVIOLET IRRADIATION OF UPPER AIR FOR THE CONTROL OF BACTERIAL AIR CONTAMINATION IN SLEEPING QUARTERS. PRELIMINARY REPORT1.” American Journal of Epidemiology 40 (2): 136–53. https://doi.org/10.1093/oxfordjournals.aje.a118981.
Shen, Jialei, Meng Kong, Bing Dong, Michael J. Birnkrant, and Jianshun Zhang. 2021. “A Systematic Approach to Estimating the Effectiveness of Multi-Scale IAQ Strategies for Reducing the Risk of Airborne Infection of SARS-CoV-2.” Building and Environment 200 (August): 107926. https://doi.org/10.1016/j.buildenv.2021.107926.
Wells, W. F., M. W. Wells, and T. S. Wilder. 1942. “THE ENVIRONMENTAL CONTROL OF EPIDEMIC CONTAGION.” American Journal of Epidemiology 35 (1): 97–121. https://doi.org/10.1093/oxfordjournals.aje.a118789.
FWIW, @Rosie_Bettle and I also found this surprising and intriguing when looking into far-UVC, and ended up recommending that philanthropists focus more on “wavelength-agnostic” interventions (e.g. policy advocacy for GUV generally)
That sounds reasonable! Thanks for adding your impression.
Hello—just catching up with this post, and signed up to ask a question:
Is there a reason that the framework for discussing using safe UV light in 2024 does not prominently concern reducing the death toll in residential nursing care and rehabilitation facilities? Most people dying of Covid these days are over 75 and unable to do without caregivers, and a very large proportion are unable to mask—certainly not 24⁄7 in their care residences. Their care-givers often can’t mask either and be understood and effective in delivering care to older people. I would think that if we knew of some other sector where 50,000 deaths were occurring each year because of Covid and flu that we be urgently looking to disinfect the air there—in those relevant spaces. I thought I read somewhere that UV light is already used in homeless shelters, and has been for years. What’s the difference?
Thanks if you have a moment to answer.
There are two separate questions here. (1) Why has society not adopted this over decades and (2) Why do EA people who promote far-UVC not also promote the old technology? The second question has a precise answer.